Head injuries can result in a wide range of complications, and among the most commonly reported are disturbances in vision. For individuals recovering from traumatic brain injuries (TBI), the sudden onset of visual problems can be alarming and disruptive to everyday life. Early recognition and proper management of these symptoms significantly enhance recovery outcomes. For those seeking support and treatment options, especially locally, learn more about solutions for blurred vision Halifax and related visual changes.
Whether the result of a sports concussion, fall, or accident, head trauma often disrupts the way the brain processes visual signals. These issues can persist if not addressed, affecting everything from reading and driving to mobility and workplace performance. According to the Brain Injury Association of America, as many as 90% of TBI patients experience visual dysfunction post-injury. Being aware of these symptoms and seeking prompt evaluation is crucial for maintaining independence and quality of life.
Common Vision Problems Post-Head Injury
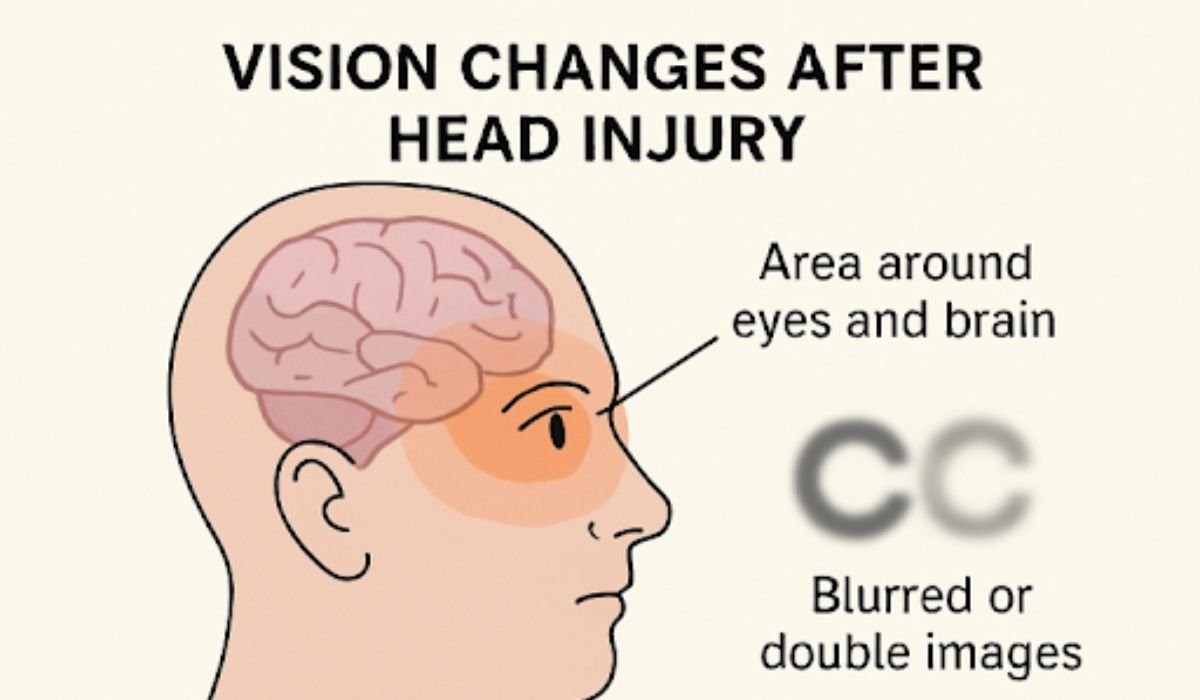
After a traumatic brain injury, people may experience an array of visual disturbances. Some of the most frequent issues include:
- Blurred or Double Vision: A common complaint, this causes objects and text to appear unclear or to overlap, leading to difficulty reading and focusing.
- Light Sensitivity: Bright environments can cause discomfort and pain, making everyday tasks challenging.
- Difficulty with Eye Movements: Trouble tracking moving objects or shifting gaze may make it hard to watch TV, drive, or cross busy streets.
- Reduced Depth Perception: Individuals may have difficulty judging distances, increasing the risk of falls, especially on stairs or curbs.
- Visual Field Loss: Losing parts of the visual field like hemianopsia (loss of half the visual field) or quadrantanopia (loss of a quarter) may go unnoticed until it impacts routine activities.
Compounding this challenge is the fact that vision disturbances are sometimes missed during initial medical evaluations for head trauma.
Underlying Causes of Vision Changes
For the eyes and brain to work efficiently, complex neural pathways must coordinate the processing of visual information. Head trauma can disrupt this coordination in several ways:
- Optic Nerve Damage: Trauma, swelling, or increased intracranial pressure can compress the optic nerve, potentially leading to vision loss or blind spots.
- Retinal Injury: Direct impact can lead to retinal tears, detachment, or hemorrhage. These changes can be sudden and require urgent attention.
- Disruption in Neural Pathways: The brain’s ability to interpret visual cues may be impaired, leading to symptoms such as fluctuating vision, spatial confusion, or even hallucinations.
Identifying the root cause is essential for proper management and customized therapy, as different injuries affect unique aspects of vision.
Diagnosis and Assessment
After a head injury, vision changes can occur and often require evaluation by both eye care specialists and neurologists. Examinations typically assess visual acuity, field of vision, and eye movements, while neurological tests can reveal cognitive or perceptual issues associated with brain injury. Imaging studies, like MRI or CT scans, may also be used to confirm trauma to the brain or optic nerves. Detecting these problems early is important, as prompt intervention can prevent long-term vision issues. Health organizations recommend routine vision screenings after significant head injuries to ensure any complications are identified and addressed quickly.
READ ALSO: The Importance of Evidence in Personal Injury Cases
Treatment and Rehabilitation
Managing visual disturbances related to head injury is rarely a one-size-fits-all process. Rehabilitation plans are most effective when tailored to the individual’s specific deficits and daily needs, and may include:
- Vision Therapy: Structured exercises and activities can retrain the eyes and brain to work together more efficiently, especially for problems with eye alignment and coordination.
- Corrective Lenses: Glasses or contact lenses, sometimes with specialized prisms, can address specific focusing or field-of-view concerns.
- Medications: Prescription eye drops or oral medications may help relieve inflammation, reduce pain, or manage coexisting neurological symptoms.
- Surgical Management: Ophthalmic surgery might be required for conditions like retinal detachment, which can occur after direct ocular trauma.
Vision therapy is supported by clinical research showing substantial improvement for concussion-related double vision and blurred vision when performed under the guidance of neuro-optometrists.
Impact on Daily Life
Visual problems after a head injury can affect many parts of daily life. Tasks like reading and writing may become harder due to trouble focusing or tracking lines, while driving can be unsafe because of reduced depth perception and limited visual fields. Even moving around at home or in the community may be challenging, and balance issues can increase the risk of falls. These changes can also impact emotional health, sometimes causing anxiety, depression, or isolation. Early and effective interventions can help improve vision and overall well-being, supporting independence and confidence in everyday activities.
Preventive Measures and Safety Tips
While not every head injury can be avoided, adopting a safety-first mindset is critical. To protect vision and minimize the risk of injury, consider these evidence-based recommendations:
- Wear Protective Gear: Helmets are a must during activities such as cycling, skiing, or construction work.
- Make Environments Safe: Clear tripping hazards from living spaces, add handrails, and ensure sufficient lighting.
- Schedule Regular Eye Exams: Post-injury check-ups are especially important, even if symptoms seem minor or have resolved.
Being proactive about preventive strategies reduces the chance of repeat incidents and supports long-term visual health.
Conclusion
Vision changes are among the most common and disruptive effects of head injuries. Understanding the connection between brain trauma and visual processing, recognizing symptoms early, and engaging in targeted therapy are essential steps for an optimal recovery. By prioritizing vision care and adopting proactive safety strategies, individuals can continue to lead independent, fulfilling lives after a head injury.
YOU MAY ALSO LIKE: How Jury Verdicts Influence Injury Settlements